by Joyce Jaixen, PT, GCS, C/NDT
When I was 14 years old, I met a boy in the grade above me who had just returned home from rehabilitation out of state, just in time for Christmas. His promising future of football and farming was disrupted by a complete T3 spinal cord injury.
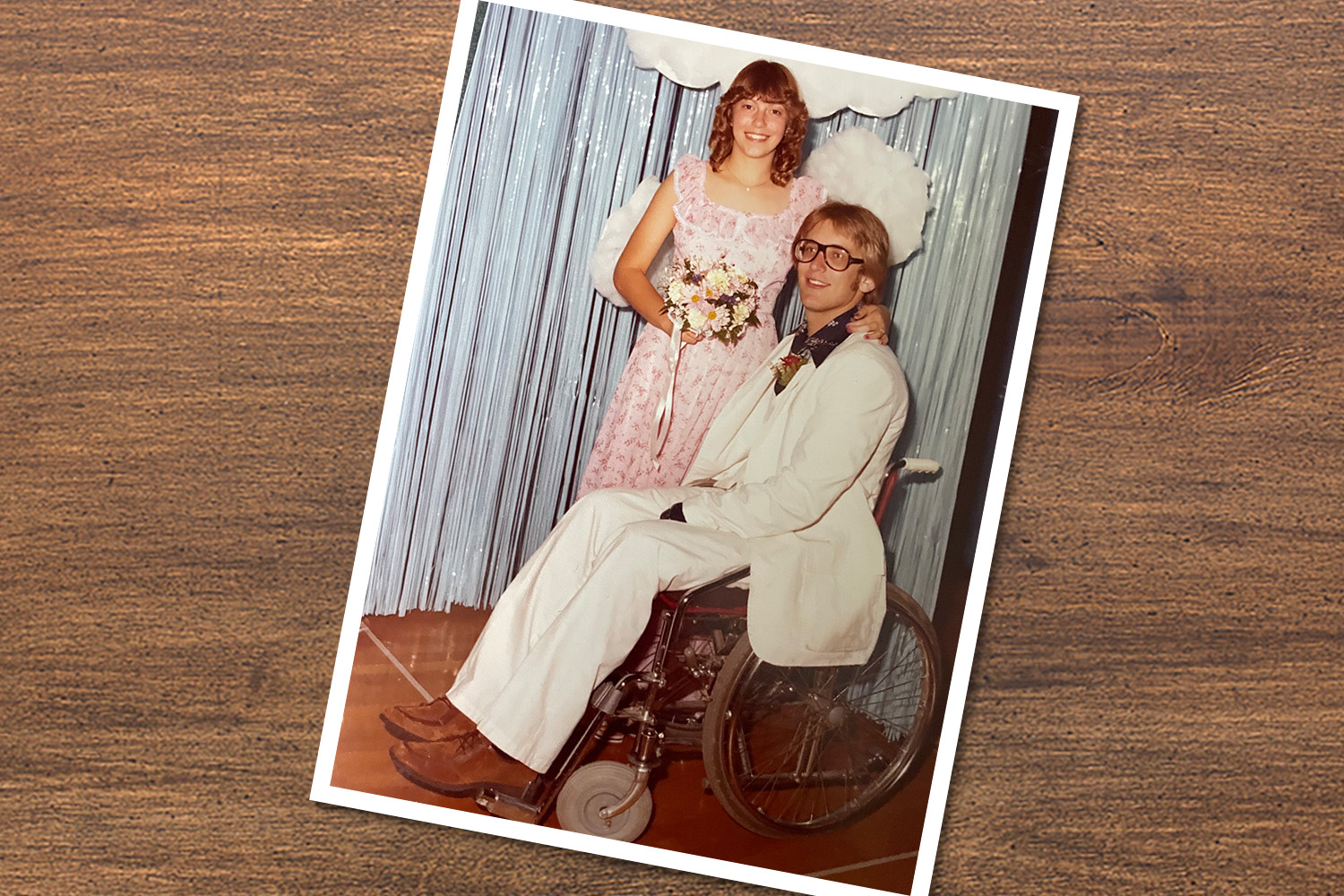
His locker was around the corner from mine; over the next few months, we became better acquainted and found ourselves paired up at the high school Sweetheart Dance. I was impressed by his ability to spin around in his wheelchair while sustaining a wheelie. I was even more impressed when he kept his balance in a wheelie for entire classic rock songs with me sitting side-saddle on his lap. I was having the time of my life and was not ready to leave the dance with my brother and girlfriend, who had driven me there.
I was excited when my date offered me a ride home, not only because we could spend more time together, but also because I was curious to know how he operated a vehicle. I observed for the first time how to go about loading and unloading a wheelchair and how to drive with hand controls. I was struck by how well this boy had adapted to a new way of moving and living in just a few months.
As he told me about his rehab therapists and how they prepared him for life in a wheelchair, I was hooked on the idea of becoming a physical therapist in a rehab setting. I was also hooked on him and was quickly introduced to his family at their farmhouse, which was adapted to accommodate his needs. I could see that his parents and three siblings also had a matter-of-fact acceptance of his condition as he went about the process of getting “back to living.”
He went on to establish a successful career, raise a family, and continue to model how to make the best of life, helping others adjust through peer volunteer work and involvement in monthly support groups for others with spinal cord injury.
Jim, now my husband of 40 years, not only introduced me to the profession of physical therapy but also showed me how key elements of social support are critical to successful outcomes.
After graduating from high school, I majored in a two-year pre-physical therapy program at a state college two hours away. My husband was employed full time as an assistant manager of a credit union in town while majoring in data processing at the community college. His family was at first nervous when he moved from the farm to establish our first home in a retirement community apartment, the only available wheelchair-accessible rental. I checked on him once or twice a week using my long-distance calling card, and drove home every weekend to plan our wedding and make goulash for him to eat through the following week. As he established new friendships in college, he remained close to his parents and siblings, all of whom were eager to assist him if needed.
Shortly after our wedding, my fiancé was recruited for employment as a software support information technologist in Salt Lake City, Utah. When offered the job, his first question was, “is there a PT school there?” I was able to transfer all my credits to the University of Utah and after completing a few extra pre-requisites was ready to apply. During my interview, I was asked a very pointed question regarding how serious I was about becoming a physical therapist. Boy, did they get an ear-full as I detailed my personal experiences with my husband as well as my experiences working part time as a physical therapy aide in two different settings before and after our move.
Upon graduation in 1987 I was offered a position at the University of Utah Physical Medicine and Rehabilitation Hospital. A few years later I was fortunate to have the opportunity to certify in Neuro- Developmental Treatment, which improved my handling of patients with neurological impairments. As we adopted four children and my husband traveled extensively and worked long hours to support us, my employment choices reflected the ever-changing needs of our family. The flexibility of the physical therapy profession enabled me to gain additional experience in home health care and school settings.
After 20 years in Utah, we moved back “home” to Nebraska to be closer to our aging parents. My draw to the rehabilitation setting led me to apply for a position at Madonna Rehabilitation Hospital in Lincoln. My decision to pursue becoming a board-certified clinical specialist in geriatric physical therapy was prompted by the high acuity of elderly patients admitted to Madonna’s Acute Rehabilitation Unit. As I prepared for the exam, I expanded my clinical reasoning skills with information provided through APTA and recommended by co-workers who had likewise obtained board certification.
My husband’s ability to calmly manage our teenage daughter’s high school drama and her younger sister’s grade school antics afforded me the time to study for the board exam while working on the Stroke Team. Nearly five years ago I transitioned to Madonna’s Therapy Plus Outpatient Intensive Rehab Day Program, where the interdisciplinary team of physical therapists and assistants, occupational therapists and assistants, a recreation therapist, a neuropsychologist, a social worker, a nurse program manager, and physicians work collaboratively to sort out the medical, social, psychological, financial, and equipment needs of patients whose medical complexity makes difficult the transition to their homes and communities.
I’m grateful for what my career in physical therapy has enabled me to do for patients over the years, but perhaps never so much as being able to help another person close to me: my mother.After surviving two hospitalizations for COVID-19 in the fall of 2021, my 85-year-old mother experienced a more recent period of falls and delirium associated with polypharmacy, a prevalent problem among elderly patients with complex medical conditions. Because of her pre-morbid Parkinson’s diagnosis, her physicians mistakenly attributed the increase in horrible vivid nightmares, fight or flight responses, subsequent falls, and intense tremors to progression of her PD.
This is where experience in movement systems analysis, treatment of neurologic impairment, and board certification as a geriatric clinical specialist really helped me to sort through her symptoms. We discovered that her rapid decline was directly related to the side effects of at least 10 different medications and an underlying urinary tract infection. Persistent advocacy for my mother to her primary care physician, her neurologist, and her psychiatrist was necessary to either eliminate or reduce the dosage of those medications and to treat the underlying infection. Once medically stable, she again embraced the hard work of physical therapy and rallied back to independent living. As I live, breathe, and promote movement as medicine, I personally and repeatedly experience the miracles of those closest to me “brought-back to life” with the help of physical therapy and the support of their loved ones.
© 2022 American Physical Therapy Association. All rights reserved. Reprinted with permission.